Everything you need to know about neuromuscular diseases

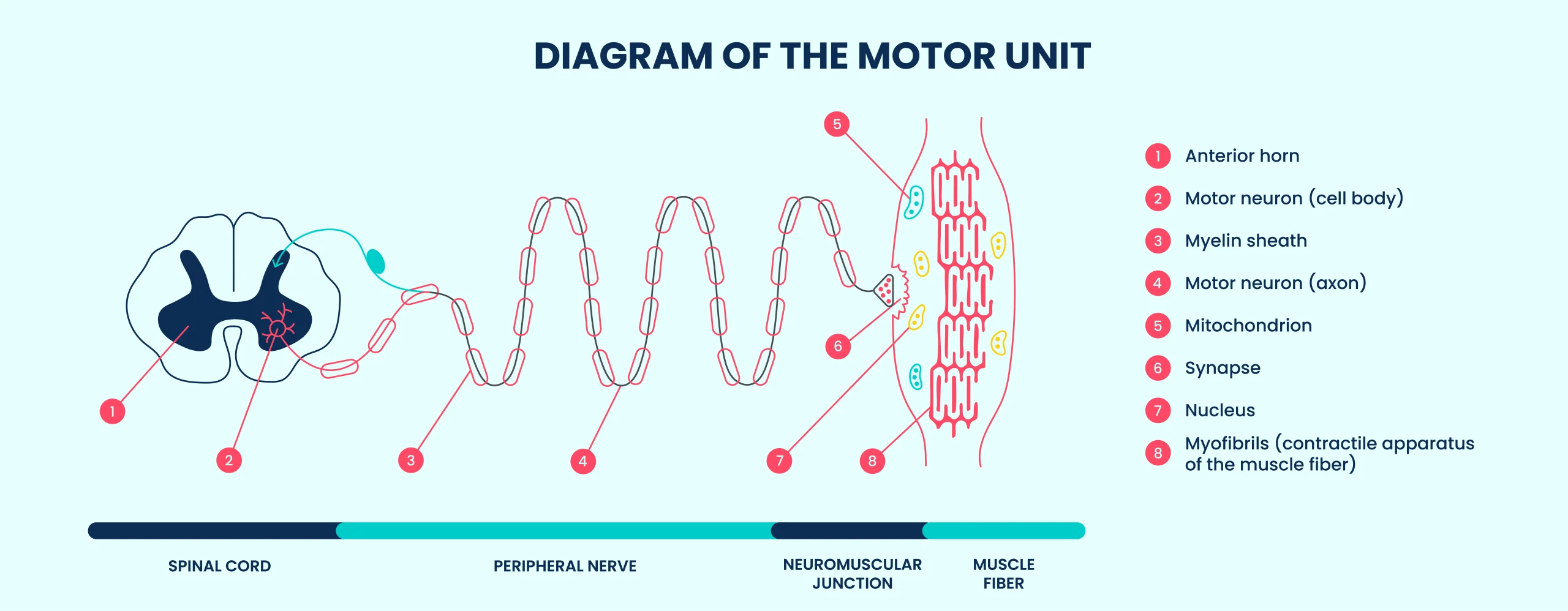
Neuromuscular diseases are a group of rare disorders that affect the peripheral nervous system. They lead to impaired motor function through various mechanisms.(1)
This motor impairment can result from damage to:
- des motor neurons (or motoneurons) or nerves
- the neuromuscular junction
- or the muscle fibers
What is a neuromuscular disease?
Definition and mechanisms of neuromuscular diseases
Neuromuscular diseases are chronic, often progressive conditions that affect the components involved in voluntary movement (including motor neurons, peripheral nerves, the neuromuscular junction, and muscle fibers). They are generally responsible for progressive muscle weakness, which may be accompanied by pain, cramps, or even paralysis.
These diseases prevent muscles from functioning properly, either because the nerves that control them deteriorate, the muscles fail to respond appropriately, or the signal between the nerve and the muscle is disrupted.(1)(3). As a result, the pathological process impairs the efficiency of movement or muscle contraction.
What causes neuromuscular diseases?
There are several possible causes of neuromuscular diseases. In some conditions, the origin lies in a genetic abnormality, this can occur spontaneously or be inherited from the parents. The mutation disrupts the transmission or execution of motor signals (at the level of the cell, nerve, or muscle), ultimately leading to disease(3).
In other cases, the immune system malfunctions and mistakenly targets specific parts of the body. This can damage the nerves (referred to as neuropathies), interfere with the signal between the nerve and muscle (as in myasthenia gravis), or cause inflammation of the muscles (known as myositis).(1)
There are also other so-called acquired causes, such as the use of certain medications or toxic substances, vitamin deficiencies, hormonal or systemic disorders, and infections.
More than 400 neuromuscular diseases exist.
Which ones are the most common?
common neuromuscular diseases
Some neuromuscular diseases are diagnosed more frequently than others:
- Duchenne/Becker muscular dystrophy: a severe genetic disorder affecting muscles, appearing in boys.(4)(5).
- Charcot-Marie-Tooth neuropathies: hereditary disorder of the peripheral nerves (the body’s “electrical wires” that transmit messages between the brain and the rest of the body).(6).
- Steinert’s myotonic dystrophy: characterized by myotonia (difficulty relaxing a muscle after a voluntary contraction), along with cardiac and endocrine complications.(7).
- Facioscapulohumeral Muscular Dystrophy (FSHD): fften begins with weakness in the muscles of the face and shoulders.(8).
Other conditions are less well known to the public, but just as impactful:
- Spinal muscular atrophy linked to the SMN1 gene: a severe genetic disorder of early infancy that affects motor neurons (the “messengers” sending movement commands from the brain to the muscles).(9).
- Mitochondrial myopathies: Involve impaired energy production within muscle cells.(10).
- Congenital myasthenic syndromes present from birth, these disorders involve defects in neuromuscular signal transmission.(11).
Symptoms of neuromuscular diseases
The nature of symptoms in neuromuscular diseasesvaries depending on the specific condition(1). However, several clinical signs are recurrent and should raise concern.
Progressive muscle weakness is the most common symptom. It may begin in the legs, arms, or facial muscles, depending on the disease.(3)
Some people also report muscle pain, unusual fatigue, or recurrent cramps. These issues can affect walking, gripping objects, or even breathing.(1)(3).
Certain conditions, such as myotonic dystrophies, have more specific symptoms, including myotonia (difficulty relaxing a muscle after contraction), cardiac problems, or early-onset cataracts.(3).
Even subtle signs can be key to diagnosis, highlighting the importance of early recognition and medical evaluation.
How is a neuromuscular disease diagnosed?
Medical examinations and genetic testing
To diagnose a neuromuscular disease, a combination of clinical and biological tests is essential.(3).
The doctor performs a neurological clinical examination and may order several specific complementary tests:
- Electromyography (EMG) measures the electrical activity of muscles.
- Muscle biopsy examines muscle cells under a microscope.
- Genetic testing identifies possible mutations responsible for the disease.
Blood tests may also reveal an elevated level of creatine phosphokinase (CPK), a marker of muscle damage.
The importance of early diagnosis
An early diagnosis enables quicker medical management and, in some cases, access to innovative treatments that can slow the progression of the disease.
It is also a gateway to participating in clinical research protocols. Additionally, it facilitates genetic counseling—a consultation with a specialist to understand whether a genetic disease may affect an individual or their family, as well as the risks of transmission.(3)(12).
Traitements et prise en charge des maladies neuromusculaires
Medication-Based approaches and emerging therapies
In recent years, innovative therapies have become available for certain neuromuscular diseases. Some help stabilize the condition, others slow down motor decline, relieve symptoms, and delay disease progression.
Several medications are already in use:
- Corticosteroids(13)(such as prednisone) are prescribed for certain forms like Duchenne muscular dystrophy. They help preserve muscle strength and delay the loss of mobility.
- Immunosuppressive treatments are used in autoimmune forms. Their goal is to reduce inflammation when the immune system mistakenly attacks the muscles.
New avenues of research are also underway:
- Gene therapies, such as exon skipping(14) or CRISPR technology(15) (a kind of “genetic scissors” that can correct DNA errors), aim to target the root cause of the disease.
- Cell therapy and certain biologic drugs are also being tested in clinical trials. The objective is to develop more targeted and longer-lasting treatments.
Rehabilitation and maintenance of motor function
Functional rehabilitation is a central pillar of patient care. Its main goals are to maintain autonomy and prevent complications.
The tools and methods used include:
- Specialized physiotherapy
- Stretching and strengthening exercises
- Orthotic devices to support weakened limbs
Depending on the severity of the condition,the use of electric wheelchairs or walking aids may be necessary(3).
Innovative solutions to improve quality of life
- Arm supports mounted on wheelchairs: these articulated systems help support and/or reduce the weight of the arms, making gestures like eating or reaching easier.
- Passive exoskeletons: these are non-powered devices made with mechanical components like springs. They assist with repetitive movements and help reduce muscle fatigue in the arms or shoulders.
- Dynamic orthoses: these supports provide stability while allowing a degree of movement, helping users perform tasks with greater ease and control.
- Robotic assistive arm: these motorized assistive arms can be mounted on wheelchairs and controlled by the user. They allow individuals to perform everyday tasks independently, such as drinking, opening doors, or picking up objects.
Many users report a significant positive impact on their autonomy and quality of life.
Neuromuscular diseases require a multidisciplinary approach that combines medicine, genetics, rehabilitation, and technological innovation. A better understanding of these conditions paves the way for more targeted and effective treatments.(3). Raising awareness, ensuring early diagnosis, and providing long-term support are the key pillars of successful management for neuromuscular diseases.
Sources
1. Anamorphik. Maladies neuromusculaires [Internet]. Fédération Française de Neurologie. 2024 [cité 2 mai 2025]. Disponible sur: https://www.ffn-neurologie.fr/maladies/maladies-neuromusculaires/
2. Centre de référence constitutif des maladies rares neuromusculaires Nord/Est/Ile-de-France – GNMH – ESMARA [Internet]. [cité 2 mai 2025]. Disponible sur: https://esmaramaladiesrares.fr/centre-de-reference-des-maladies-rares-neuromusculaires-gnmh/
3. Maladies neuromusculaires | AFM Téléthon [Internet]. 2020 [cité 2 mai 2025]. Disponible sur: https://www.afm-telethon.fr/fr/fiches-maladies/maladies-neuromusculaires
4. Dystrophie musculaire de Duchenne | AFM Téléthon [Internet]. 2024 [cité 2 mai 2025]. Disponible sur: https://www.afm-telethon.fr/fr/fiches-maladies/dystrophie-musculaire-de-duchenne
5. Dystrophie musculaire de Becker | AFM Téléthon [Internet]. 2024 [cité 2 mai 2025]. Disponible sur: https://www.afm-telethon.fr/fr/fiches-maladies/dystrophie-musculaire-de-becker
6. Maladie de Charcot-Marie-Tooth | AFM Téléthon [Internet]. 2024 [cité 2 mai 2025]. Disponible sur: https://www.afm-telethon.fr/fr/fiches-maladies/maladie-de-charcot-marie-tooth
7. Maladie de Steinert | AFM Téléthon [Internet]. 2020 [cité 2 mai 2025]. Disponible sur: https://www.afm-telethon.fr/fr/fiches-maladies/maladie-de-steinert
8. Myopathie facio-scapulo-humérale | AFM Téléthon [Internet]. 2024 [cité 2 mai 2025]. Disponible sur: https://www.afm-telethon.fr/fr/fiches-maladies/myopathie-facio-scapulo-humerale
9. Amyotrophie spinale proximale liée à SMN1 | AFM Téléthon [Internet]. 2025 [cité 2 mai 2025]. Disponible sur: https://www.afm-telethon.fr/fr/fiches-maladies/amyotrophie-spinale-proximale-liee-smn1
10. Myopathies mitochondriales | AFM Téléthon [Internet]. 2024 [cité 2 mai 2025]. Disponible sur: https://www.afm-telethon.fr/fr/fiches-maladies/myopathies-mitochondriales
11. Syndromes myasthéniques congénitaux | AFM Téléthon [Internet]. 2020 [cité 2 mai 2025]. Disponible sur: https://www.afm-telethon.fr/fr/fiches-maladies/syndromes-myastheniques-congenitaux
12. La consultation de conseil génétique | AFM Téléthon [Internet]. 2014 [cité 2 mai 2025]. Disponible sur: https://www.afm-telethon.fr/fr/vivre-avec-la-maladie/je-m-informe-sur-les-maladies/comprendre-les-maladies-genetiques/consultation-genetique
13. Manuels MSD pour le grand public [Internet]. [cité 2 mai 2025]. Table:Corticoïdes : Utilisations et effets secondaires. Disponible sur: https://www.msdmanuals.com/fr/accueil/multimedia/table/corticoïdes-utilisations-et-effets-secondaires
14. Goyenvalle A, Vulin A, Fougerousse F, Leturcq F, Kaplan JC, Garcia L, et al. Le saut d’exon thérapeutique : un espoir pour les dystrophinopathies. médecine/sciences. 1 déc 2004;20(12):1163‑5.
15. CRISPR-Cas9 : une avancée pour les maladies génétiques | AFM Téléthon [Internet]. 2025 [cité 2 mai 2025]. Disponible sur: https://www.afm-telethon.fr/fr/termes/crisprcas9